Retinopathy, a term often heard in the realm of ophthalmology, refers to a condition that affects the retina – the light-sensitive tissue at the back of our eyes. It encompasses a range of disorders that can lead to vision impairment or even blindness if left unmanaged. Among the various causes, diabetes is a primary culprit when it comes to the development of retinopathy. The correlation between diabetes and retinopathy has prompted the establishment of diabetic eye screening programs, aimed at detecting and managing this sight-threatening condition. In addition, retinopathy shares common ground with another prevalent eye disease – glaucoma – both of which demand careful attention and understanding for effective treatment strategies. In this article, we venture into the world of retinopathy, aiming to shed light on its causes, symptoms, screening methods, and the crucial role of early intervention in preserving vision. Let us embark on this enlightening journey through the looking glass of retinopathy.
The Connection Between Diabetes and Retinopathy
Check It Out
Diabetes and retinopathy have a close relationship. In fact, retinopathy is one of the most common complications of diabetes, particularly for individuals who have been living with diabetes for several years. Retinopathy occurs when the blood vessels in the retina, which is the light-sensitive tissue at the back of the eye, become damaged.
People with diabetes are at a higher risk of developing retinopathy due to the chronic high levels of blood sugar. Over time, these elevated levels can cause damage to the small blood vessels in the retina, leading to various changes and impairments in vision.
Regular diabetic eye screening is crucial for early detection and management of retinopathy. By detecting retinopathy at an early stage, appropriate measures can be taken to prevent further damage and preserve vision. This is why individuals with diabetes are encouraged to undergo regular eye examinations to monitor the health of their eyes and identify any signs of retinopathy or other eye diseases such as glaucoma.
Remember, when it comes to diabetes and retinopathy, early detection and proactive management are key to maintaining optimal eye health.
Understanding Diabetic Eye Screening
- The Importance of Diabetic Eye Screening
Diabetic eye screening is a crucial aspect of ophthalmology for individuals with diabetes. This screening process plays a significant role in detecting and monitoring the development of retinopathy. This condition, associated with diabetes, affects the blood vessels in the retina and can ultimately lead to vision loss if left untreated. Diabetic eye screening aims to identify retinopathy at an early stage, allowing for timely intervention and management to prevent further complications.
- The Process of Diabetic Eye Screening
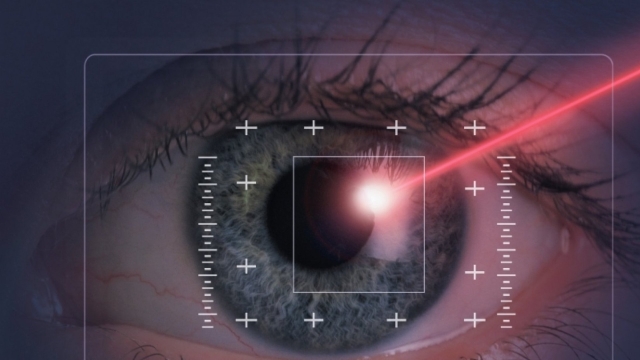
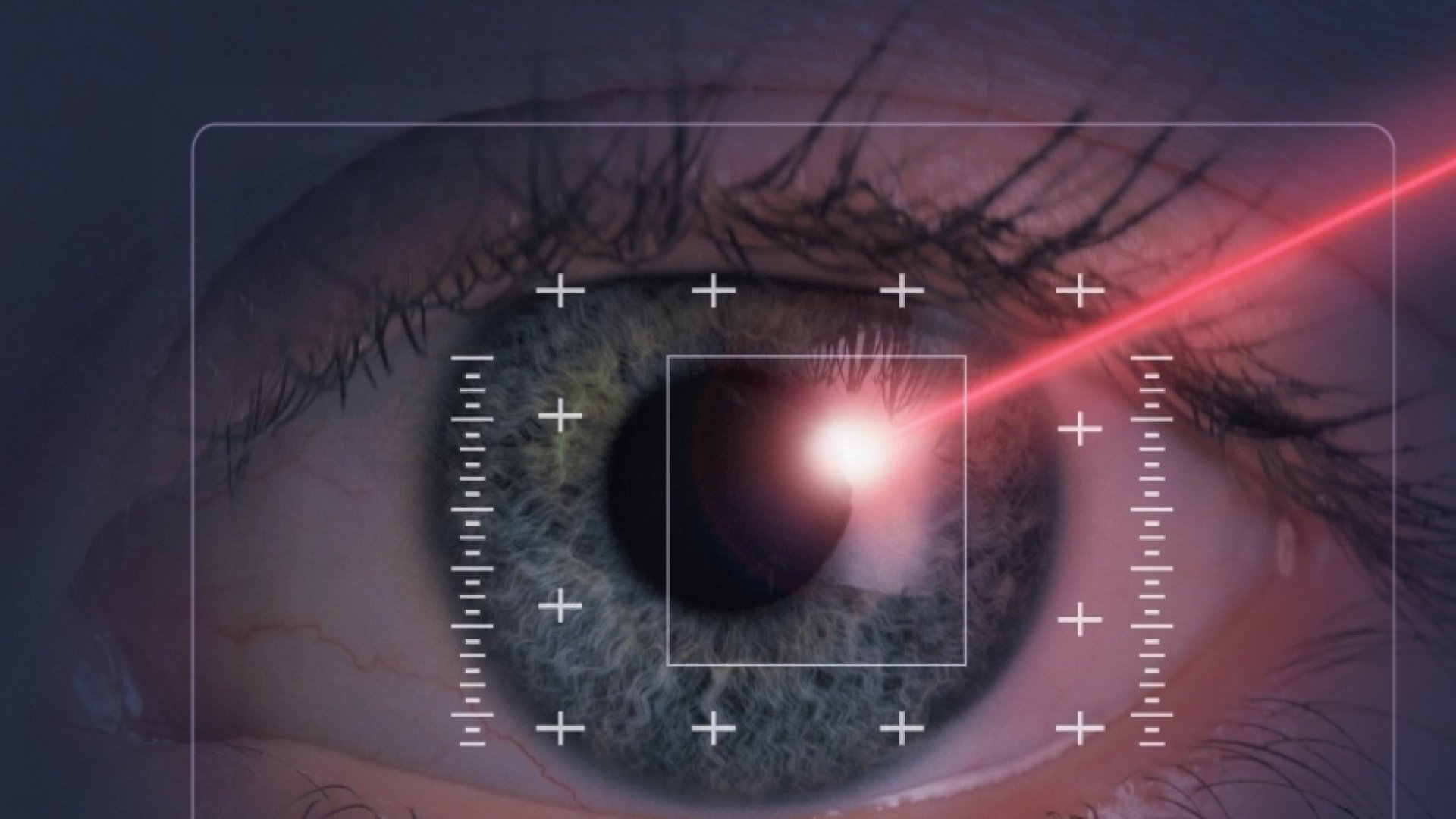
During a diabetic eye screening, a trained healthcare professional will carefully examine the eyes using specialized equipment. Typically, this involves capturing high-resolution images of the retina, which can further be analyzed for any signs of retinopathy. This procedure is non-invasive and painless, making it accessible and comfortable for individuals. Regular screenings are recommended to ensure the early detection of retinopathy, as its presence might not always be accompanied by noticeable symptoms.
- Diabetic Eye Screening and Beyond
While diabetic eye screening primarily focuses on detecting and monitoring retinopathy, it also serves as an opportunity to assess other eye conditions such as glaucoma. Glaucoma is an eye disease that damages the optic nerve, leading to gradual vision loss. By incorporating glaucoma assessments into the screening process, healthcare professionals can identify and address potential vision-related concerns comprehensively. Together, these screenings contribute to the overall well-being of individuals with diabetes, promoting early intervention and enabling optimal eye health management.
The Link Between Retinopathy and Glaucoma
Retinopathy and glaucoma are two interconnected eye conditions that often coexist and can have a significant impact on one’s vision and overall eye health. Understanding the relationship between these conditions is crucial in order to effectively manage and provide appropriate care for patients.
Retinopathy, a common complication of diabetes, is the condition in which the blood vessels in the retina, the light-sensitive tissue at the back of the eye, become damaged. This damage can lead to vision problems and, in severe cases, even blindness. Regular ophthalmology check-ups and diabetic eye screening are essential for early detection and intervention, as untreated retinopathy can worsen over time.
Glaucoma, on the other hand, is a group of eye diseases characterized by damage to the optic nerve, often caused by increased pressure within the eye. It is a leading cause of irreversible vision loss worldwide. Interestingly, studies have shown a potential association between retinopathy and glaucoma. The presence of retinopathy in diabetic patients has been found to increase the risk of developing glaucoma. Additionally, individuals with glaucoma may also have an increased likelihood of developing retinopathy.
The exact mechanism behind this link is not fully understood, but it is believed that the common underlying factors such as diabetes, high blood pressure, and genetics, may contribute to the development of both conditions. Managing these conditions requires a comprehensive approach that involves close collaboration between ophthalmologists and other healthcare professionals to monitor and treat both retinopathy and glaucoma, thereby minimizing the potential for vision loss.
Understanding the connection between retinopathy and glaucoma is crucial for early detection, timely intervention, and effective management of these eye conditions. Regular eye screenings, lifestyle modifications, and adherence to treatment plans are essential in preserving vision and maintaining overall eye health. By staying informed and proactive, individuals can take steps to mitigate the impact of these conditions and optimize their eye health outcomes.